President's Desk
Legends in Neuropathology

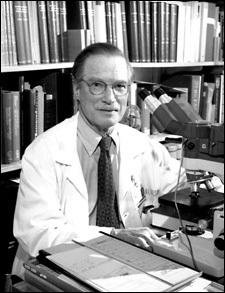
DENNIS W DICKSON
My dear Friends and Colleagues, During the past 10 months, I have been communicating with you all once in a month .I sent a series on Legends in Neuropathology. I am sure you would have read all these ‘write-ups’ and found some useful information. Last in this series...

DR. HANS A KRETZSCHMAR
December 5, 2017 Dear Members, I am sure that most of you would be enjoying early winter nowadays. The weather in ‘God’s own country’ is still warm but quite pleasant in nights. I am sending herewith the next ‘write-up’. I do hope it will make an interesting reading...

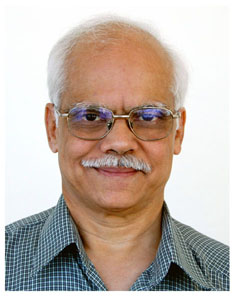
Prof. Subimal Roy( 1933- 2015)
November 1, 2017, Dear member, I am sure you are reading the series on- Legends in Neuropathology. I would very much appreciate to hear or see any messages from you on this subject. This time I am sending the write-up on Prof.Subimal Roy, founder president of our...
DARAB K DASTUR (1924-2000)
October 6, 2017 My dear Friends, It is a festival time in most parts of our country. The festival of lights (Deepawali) is around the corner. I send my best wishes to you and your family on this occasion and also pray to Almighty to bless you all with happiness and...

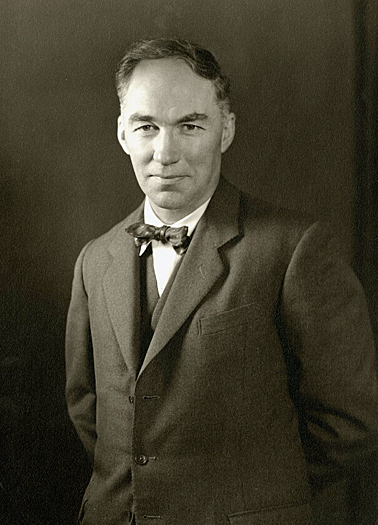
Harry M. Zimmerman MD (1901-1995)
August 30, 2017 Dear friends and colleagues It is the festival time in God’s own country!!. The ‘Onam’ festival season has already begun here in great festive mood. This is the time when King Mahabali visits us and wishes to see his people in a happy frame of mind and...

Bernd W. Scheithauer, MD (1946–2011)–Mentor, Friend, and Prodigy
August 1, 2017. My dear colleagues, In continuation on the series- ‘Legends in Neuropathology’, I am sending herewith a ‘write-up’ on BW Scheithauer- Mentor, Friend and Prodigy. So far I did not find comments to any one of my earlier ‘write-ups’. Hence I would urge...
RAYMOD D ADAMS (1911-2008)
July 4, 2017. Dear colleagues, Greetings to you all from Thiruvananthapuram!! I am sure by now most of you would be enjoying the rainy season that is currently in full swing and must be getting respite from hot and sultry climatic conditions in particular northern...
Prof. Edward Pierson Richardson, Jr. (1918-1998)
June 8, 2017 Dear colleagues, Greetings to you all from God’s own country!! The south-west monsoon arrived here about a week with plenty of rains. Currently it is progressing towards the rest of the country. I am sure some of you will be already enjoying the rains by...
Lucien J. Rubinstein: Enduring Contributions to Neuro-Oncology
Dear colleagues and friends, Greetings to you all from God’s own country!! I do hope that most of you would have read the first ‘write-up’ on Legends in Neuropathology. In continuation with that I am sending the second ‘write-up’ on Professor Lucien J Rubinstein. I...

DORATHY STUART RUSSELL (1895-1983) –“An unconquered Queen”
Dorothy Stuart Russell born at Sydney, Australia in 1895.She lost her parents, when she was only 8 years of age. Thereafter, Dorothy and her younger sister Patronella were brought to England by her aunt and uncle living near Cambridge, England. In 1909, Dorothy...